Hemorrhoids Surgery: What are the Possible Complications?

Hemorrhoids are swollen veins, either inside the rectum (internal) or outside the rectum (external). Although they can be painful and uncomfortable, most hemorrhoidal flare-ups will stop hurting within two weeks without treatment.
The American Society of Colon and Rectal Surgeons (ASCRS) recommends that you make some lifestyle changes to manage your symptoms. This includes eating a high fiber diet and drinking 8 to 10 glasses of water per day, to help promote softer, more regular bowel movements.
It may also be necessary to use stool softeners to reduce straining during bowel movements, as straining can worsen hemorrhoids. In most cases, less than 10% of cases require hemorrhoids surgery.
In the rare instance that surgery is necessary, this is usually done when external or prolapsed hemorrhoids become too irritated, infected, or when there are complications. If you are suffering from hemorrhoids, it’s important to remember that the majority of cases will not require any medical intervention.
By making small changes to your lifestyle and focusing on promoting softer, more regular bowel movements, you can usually manage your symptoms without requiring hemorrhoids surgery.
If you are concerned about your symptoms or would like to learn more about how to manage them, contact your doctor or healthcare provider. They will be able to advise you on the best treatment option for your individual situation.
What are the Potential Risks of Hemorrhoidectomy?
When considering a hemorrhoidectomy, it is important to understand the potential risks and complications that may arise. A hemorrhoidectomy is a surgical procedure used to remove hemorrhoids, which are swollen veins in the anal and rectal area.
Although it is generally a safe and effective procedure, it does involve some rare general risks and complications. These may include:
- Anesthesia reaction: Anesthesia is used during the procedure and can cause allergic reactions, as well as issues with breathing.
- Bleeding: The surgery may cause bleeding, which can lead to shock.
- Blood clot: A deep vein thrombosis (a blood clot) may develop in the leg or pelvis, and can travel to the lungs, causing a pulmonary embolism.
- Infection: Infections can occur during and after the procedure.
What are the Potential Complications of Hemorrhoidectomy?
Similarly, these are uncommon, but the potential specific complications of hemorrhoidectomy include:
- Anal stricture: This is a narrowing of the anal canal that can occur after the procedure.
- Difficulty urinating or urinary retention: This occurs when the bladder does not empty completely.
- Fecal impaction: This is when hard stool becomes trapped in the anal canal.
- Fecal incontinence: This is when a small amount of stool leaks out uncontrollably.
- Pain with bowel movements: This is common after the procedure.
- Recurrence of hemorrhoids: The risk of the hemorrhoids returning is higher than with other treatments.
It is important to discuss all of the risks and complications of a hemorrhoidectomy with your doctor before deciding to have the procedure. Your doctor can provide information on the likelihood of these risks and complications occurring, as well as any steps you can take to reduce them.
Overall, a hemorrhoidectomy is a safe and effective treatment for hemorrhoids. Your doctor can help you make an informed decision about whether this procedure is right for you.


 Dental Crowns –Restoring Strength, Function, And Aesthetics.
Dental Crowns –Restoring Strength, Function, And Aesthetics.  One-Person Wonder: Making Waves in the Massage Industry in Gunma
One-Person Wonder: Making Waves in the Massage Industry in Gunma  How Cataract Surgery in Nashville Improves Vision and Quality of Life
How Cataract Surgery in Nashville Improves Vision and Quality of Life  Maintaining Oral Health: The Role of Dentists in Richmond
Maintaining Oral Health: The Role of Dentists in Richmond  How to Choose the Best Implant Dentist in Sheffield: A Guide
How to Choose the Best Implant Dentist in Sheffield: A Guide 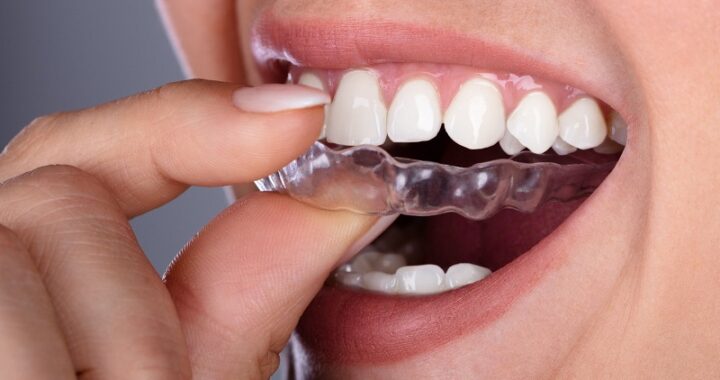 How Invisalign is Revolutionising Orthodontics in London
How Invisalign is Revolutionising Orthodontics in London  Veneers: A Popular Cosmetic Solution for a Beautiful Smile in London
Veneers: A Popular Cosmetic Solution for a Beautiful Smile in London